The only thing that stood between Dr. Johan Hultin and a mass murderer was a pair of pruning shears. Fate—or at the very least an uncanny series of coincidences—had brought him across thousands of miles and half a century to a confrontation on the frozen edge of the world. He took one last look around the desolate, deserted Alaskan landscape. Then, alone and at the age of 73, Hultin picked up his wife's garden shears and jumped into an open grave.
On that gray, dreary day in 1997, a few months before a strange and lethal outbreak of avian flu in Hong Kong threw the world into a panic, Hultin, 51MS, 53MD, uncovered a mass grave that contained victims of a much deadlier influenza pandemic. Estimates of the number of people who died worldwide during the Spanish Flu of 1918 range from 20 to 100 million. In a few short months, more Americans died from that particularly virulent form of influenza than in battle during both World Wars, the Korean War, and the Vietnam War.
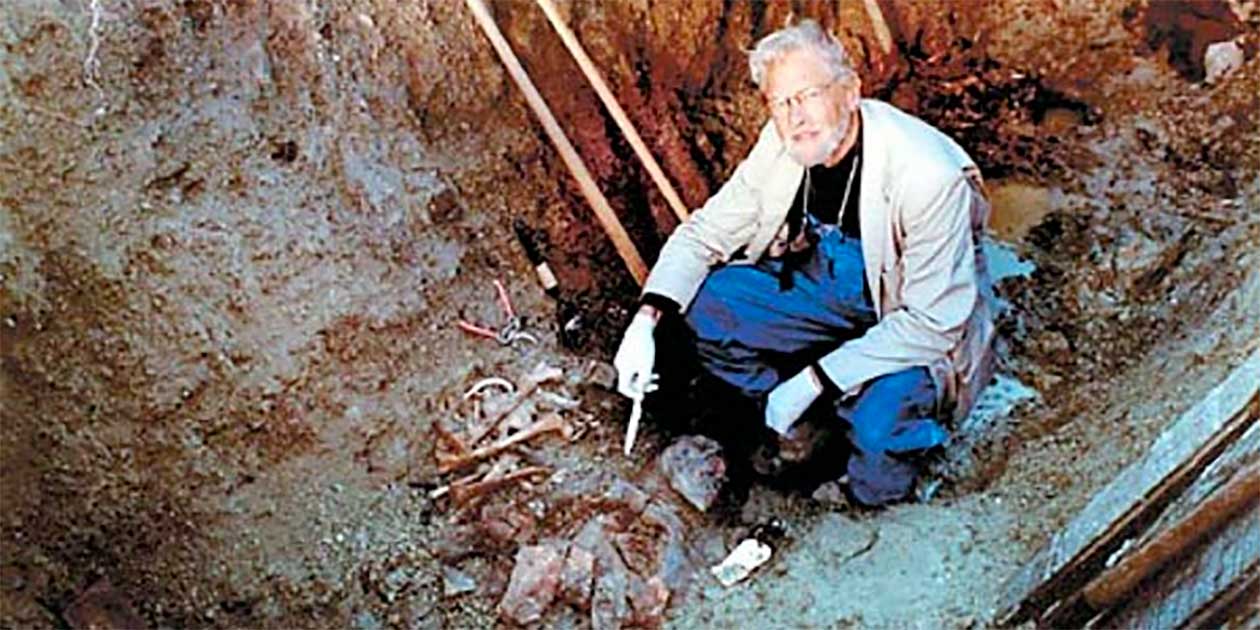 PHOTO COURTESY Johan Hultin
Determined to solve a medical mystery, Johan Hultin retrieves 1918 flu pathogens from victims of the disease.
PHOTO COURTESY Johan Hultin
Determined to solve a medical mystery, Johan Hultin retrieves 1918 flu pathogens from victims of the disease.
Of the 80 inhabitants in the tiny Alaskan community of Brevig Mission, 72 perished. Young and old, frail and hearty, they succumbed to the virus that came out of nowhere and could kill within hours. Hultin wanted to ensure their deaths were not in vain. On a secret mission to help researchers at the Armed Forces Institute of Pathology crack influenza's genetic code, the retired pathologist made the 2,600-mile trip from his home in San Francisco to the remote outpost near the Bering Straits. Among the few items he carried was a pair of pruning shears he'd purloined from his wife's gardening tools. He would use these shears to cut open the ribcages of the dead and retrieve lung tissue that might still harbor fragments of the flu virus.
Hultin's low-key, low-cost mission—which he paid for with $3,200 of his savings—was in stark contrast to a highly publicized million-dollar expedition under way at the same time in Norway. There, an extensive international team of virologists, microbiologists, infectious diseases specialists, and other experts attempted to recover samples from the bodies of seven young miners who'd died during the 1918 outbreak. Hultin may have seemed the underdog in this scientific contest, but he was uniquely placed to succeed. He knew exactly where and how to locate some of the few remaining known samples of the 1918 flu virus. He'd already been to Brevig Mission, thanks to coincidence—or maybe even destiny.
Mere chance had brought Hultin to Iowa from his native Sweden in the 1940s. At the UI, he studied microbiology, choosing influenza as the subject for both his master's and doctoral theses. One day in 1950, he happened to attend a lunch with a visiting expert virologist, who remarked that the only hope for discovering the cause of the 1918 flu was if someone could retrieve tissue from the frozen bodies of victims. For Hultin, time seemed to stand still. He realized that he'd already crossed paths with the influenza virus.
Just the previous summer, Hultin had worked with a paleontologist in a remote part of Alaska. That local knowledge, combined with his research skills and contacts with influenza experts at the UI, made him uniquely qualified for the task. In 1951, Hultin, along with his faculty adviser, virologist Albert McKee, 41MD, and a UI pathologist, Jack Layton, 43MD, flew to Alaska. There, they met Otto Geist, the paleontologist Hultin had worked with previously. It was a wild journey to an untamed frontier—the perfect setting for a daredevil mission.
Still eight years from statehood, the territory of Alaska was raw and filled with promise. The adventurers had to find a bush pilot willing to fly them to the remote villages and land a plane precariously on thin strips of shale next to the icy sea. Then they had to traipse miles across boggy terrain, hauling supplies and rudimentary scientific equipment. The weather was cold and rainy that June, but it didn't deter the swarms of mosquitoes. "The villagers thanked us for coming to help feed the mosquitoes," recalls Hultin.
Even with temperatures in the 50s, the permafrost was still frozen—and the bodies of the flu victims lay six feet below the surface. Hultin lit fires to soften the ground enough to make a dent in the rock-hard surface. For all the scientists knew, the lethal virus was still potent—but it was a risk they were willing to take. Face masks were their only protection against any surviving pathogens. Black-and-white photos taken on that expedition show the four men standing up to their shoulders in the open grave. A stark wooden cross leans lopsidedly behind them and forbidding storm clouds press down on the featureless tundra. In this bleak scene, the men's faces glow with a mixture of hope and victory.
Their excitement proved premature. Even though they managed to recover tissue samples, that first expedition to Brevig ultimately failed. During weeks of experiments back in his UI laboratory, Hultin couldn't manage to grow the virus. Though potentially deadly, the influenza virus is strangely fragile; just an hour's exposure to room temperature can destroy it. After all those years in the ground, the pathogens were dead.
Hultin never did complete his doctoral thesis on the influenza virus. Instead, he entered medical school at Iowa, eventually becoming a successful pathologist in California. But, all along, he couldn't shake the feeling that influenza wasn't done with him. He was right.
"Influenza is the most realistic threat to humankind. It's already—in 1918—been the most virulent killer in human history."
More than four decades later, Hultin read about the work being done by Jeffery Taubenberger of the Armed Forces Institute of Pathology, using a few tissue samples from soldiers who had died in the 1918 flu pandemic. He knew that advances in molecular biology gave scientists a much better chance of piecing together the puzzle of the lethal pathogen. Out of the blue, he sent Taubenberger a letter offering to return to Alaska and gather more tissue samples. Taubenberger was skeptical at first, until he saw Hultin's professional credentials and found out about his experiences in Alaska. Thinking of the Norway expedition that took several years to plan, he asked when Hultin could start. "I apologized and said that I couldn't leave that week," remembers Hultin, "but I could go the week after."
The long journey to Alaska was less arduous than his first expedition all those years ago, but the stakes were much higher. Influenza typically appears in 30-year cycles. Since the 1918 outbreak, only two smaller epidemics—the "Asian Flu" in 1957 and the "Hong Kong Flu" of 1968—have occurred. Another pandemic was overdue, and time was running out. "Influenza is the most realistic threat to humankind," says Hultin. "Not overpopulation or a nuclear war or terrorists, but Influenza Type A. It's already—in 1918—been the most virulent killer in human history."
At a hastily convened meeting of the Brevig Mission council, Hultin convinced the villagers that the virus posed no risk and that great good could come of his endeavor. Luckily, the village matriarch, whose relatives had died from the flu, remembered Hultin from his first visit. Later, the pastor of the Lutheran church told Hultin that he was the only person who could have convinced the villagers to give up their dead.
Within hours of that meeting, Hultin was back at the graveside. By another stroke of luck, he uncovered the well-preserved corpse of an obese woman whose layers of fat had insulated her internal organs against the permafrost's occasional thaws. Hultin named her Lucy, after the famous prehistoric female discovered in Africa in 1974. "Lucy is from the Latin word 'lux,' for light," he explains. "African Lucy shed light on human evolution. I gave this lady the same name, knowing that she could potentially shed light on the mysteries of the 1918 flu pandemic."
The pruning shears snipped easily through Lucy's old bones, and Hultin quickly placed slices of her lungs in preserving fluid. Mission accomplished, he was ready to return home. But first, the keen amateur woodworker toiled through the night to rebuild the two large crosses that had originally marked Brevig's mass grave. In the morning, he planted the crosses in the shale, stood over the closed grave one last time, and bade farewell to the scene of death and triumph.
Back in San Francisco, he waited on tenterhooks until Taubenberger confirmed the samples contained genetic fragments of the virus. "That was one of the greatest moments of my life," he says.
In an interview with the San Francisco Chronicle, Taubenberger said, "When [Hultin] wrote and said he would try to get more samples, it hardly seemed possible …. It was incredible that he was able to do all this. [He's] an amazing man, an inspiration to us."
Hultin's part in the remarkable detective story was finally over. "So much could have gone wrong," he says. "After 55 years, everything came together. Coincidence after coincidence after coincidence; it's like I was meant to find the virus."
When he looks back on these events, Hultin admits they sound like a work of fiction. In fact, they warranted several chapters in a best-selling work of nonfiction, Gina Kolata's book Flu: The Story of the Great Influenza Pandemic of 1918 and the Search for the Virus That Caused It. Kolata calls Hultin "the Leif Erikson of the 1918 flu." Dr. Michael Apicella, chair of the microbiology department at the University of Iowa, says Hultin is "like Indiana Jones."
Hultin's middle name is Viking, and he's filled with the same fierce spirit of adventure as his ancient forebears. With his shock of white hair and deep-set piercing blue eyes, his Scandinavian heritage is evident in every bone of his tall, wiry body, as well as in the carefully measured cadence of his speech. Despite his achievements in helping solve one of the greatest medical mysteries of all time, this recipient of the Carver College of Medicine Distinguished Alumni Award is no glory hound.
"The reconstruction of the 1918 virus is due to three parties," he says. "The Eskimos gave permission to open the grave, I did my best to find a good specimen, and the researchers did the complicated stuff. I'm pleased to have played a small part in this great story, and I'm grateful for the Iowa education that helped me succeed. You can trace the story of the reconstruction of the 1918 flu virus all the way back to the microbiology lab at the University of Iowa."
Now, almost ten years after he retrieved those vital samples, Hultin's achievement has assumed even greater significance. Researchers in Taubenberger's laboratory have discovered a chilling fact about the 1918 pandemic. Even this most recent installment in the saga shares a connection to the University of Iowa. Raina Lourens, who worked for two years in Taubenberger's lab, is now a second-year medical student at the UI. After deciphering and then recreating the genetic code from Hultin's samples, Lourens and the other researchers discovered that the virus was a mutated form of bird flu. The discovery was made public in October 2005, at the same time a new outbreak of bird flu began spreading rapidly across the globe.
Once again in the media spotlight, besieged by journalists from TV and radio stations, local newspapers and the nationals, Hultin patiently repeated his story. How it will end, he doesn't know. On the day of his CNN interview, he read that bird flu had spread from Asia and Russia to Turkey. A few days later, when he got off the phone with a Wall Street Journal reporter, the virus had reached Greece and Romania. By late October, the virus—or culls to try to prevent it—had killed hundreds of thousands of birds. While the infection didn't appear easily transmissible from human to human, that could easily change—with dire consequences.
Hultin is convinced that the killer he tracked down in Alaska is stirring to life again. He and his wife, Eileen, have stocked up on the antiviral drug Tamiflu, which may offer some protection against bird flu, and they plan to get their flu shots. He's stoical and matter-of-fact about the risk of a pandemic. "Influenza has been around as long as mankind," he says. "It will come again—and soon. It's a matter of when, not if."
As he wraps up the interview for this article, Hultin is preparing for another journey—not to the frozen north, but to the balmy Mediterranean on an educational cruise with his wife. In the midst of fear and uncertainty, life goes on. The man who captured the worst killer in human history simply waits to see if destiny will throw them together again.
The UI and the Flu
 PHOTO: UI College of Public Health
As part of a College of Public Health course on zoonotic diseases, researchers collect a blood sample from a small mammal. An estimated 75 percent of emerging infectious diseases, such as bird flu, are due to zoonotic pathogens that cross from animals to humans.
PHOTO: UI College of Public Health
As part of a College of Public Health course on zoonotic diseases, researchers collect a blood sample from a small mammal. An estimated 75 percent of emerging infectious diseases, such as bird flu, are due to zoonotic pathogens that cross from animals to humans.
"The campus was under strict military police, and no one from president to sweep was allowed to enter or leave the campus without a pass.... It is due to the efficient measures that were taken to control the epidemic that the number of deaths fell well below normal."
With those chilling words in November 1918, the Iowa Alumnus magazine reported the effects of the Spanish Flu pandemic on the UI. Thirty-eight people in the university community died either from the flu or from pneumonia brought on by it. Today, experts on campus are working on a number of projects to understand the disease and prevent further pandemics.
- At UI Hospitals and Clinics (UIHC), researchers are testing whether diluted doses of influenza vaccine are effective. Apart from helping overcome vaccine shortages, this new approach is also less painful than a typical flu shot. Instead of being injected into muscle, the diluted vaccine is delivered under the skin, where the greater number of immune cells should prompt a better flu-fighting response.
- In the College of Public Health, researchers at the Center for Emerging Infectious Diseases (CEID) are conducting a two-year study of some 800 agricultural workers from across Iowa to help determine the prevalence of and risk factors for "zoonotic Influenza A"—cross-species infection from poultry or swine to humans.
- To help understand how bird flu is transmitted to humans and to develop possible vaccines, another CEID researcher is analyzing blood samples of Department of Natural Resources workers and duck hunters to see whether they have been exposed to the virus.
- Every year during flu season, Hygienic Laboratory staff monitor for new strains of influenza or "hotspots" of the disease that occur in Iowa.
- A research team from the Tippie College of Business and the Carver College of Medicine is testing whether the Iowa Electronic Markets can predict influenza outbreaks.
- This fall, as part of its preparedness plans for a pandemic, UIHC began a mass vaccination campaign of its healthcare staff. As well as preventing staff from contracting and transmitting flu, the project aimed to test the hospital's ability to quickly vaccinate a large number of people.
The Making of a Monster
It's like finding out that your mild-mannered neighbor leads a secret life as the BTK killer.
For many Americans, flu is a familiar, and not particularly worrying, disease. Every year, flu season rolls around; and, every year, the virus's worst consequences are usually reserved for the very old or the very young. Typically, about 36,000 Americans die annually from influenza. Anyone else who catches it endures a few weeks of fever, sore throat, cough, and muscle aches. Until bird flu raised its head in humans, most of us probably didn't consider influenza a deadly disease. By conservative estimates, though, a bird flu pandemic could kill 12 million people worldwide.
The virus responsible for such mayhem is a Jekyll and Hyde character. It changes and adapts, leaving scientists one step behind as they try to second-guess an invisible enemy. To prepare the annual flu vaccines, experts survey the strains that predominate one year and then try to predict which ones will appear the following flu season. Even if they guess correctly, producing a vaccine—from identifying the strain to manufacturing and distributing supplies—takes about 40 weeks.
With fears of a bird flu pandemic running high this fall, the chances of being able to manufacture enough vaccine specifically for that virus appear to be slim. Although a prototype has been developed, 12 times as much vaccine as usual is required to develop a protective immune response. To complicate matters, vaccines are usually grown in chicken eggs. Since bird flu is lethal to chickens, manufacturers have to use less virulent strains of the vaccine during the manufacturing process. A quicker method of growing vaccines in cell lines rather than eggs is being developed, but in the meantime, experts hope that the regular vaccine will offer some protection against bird flu, should an outbreak occur.
"There's a sense that we've conquered infectious diseases," says Dr. Pat Winokur, 88R, 91F, a UI associate professor of internal medicine who's conducting trials on the effectiveness of diluted flu vaccine. "But antibiotics aren't working as well as they used to against a lot of diseases, and then we get completely new viruses, such as Severe Acute Respiratory Syndrome (SARS) that appeared in 2003. Now, we're watching the natural progression of a new pandemic."

